Comment:
This study presents a provocative and counter-intuitive finding that directly challenges the conventional wisdom surrounding soy and prostate cancer. While many previous studies have suggested a protective role for soy, this large, prospective Japanese cohort finds the opposite: the highest intake of soy foods was associated with a 76% increased risk of prostate cancer mortality.
However, a closer look at the summary reveals critical nuances that must be understood before drawing any simple conclusions.
-
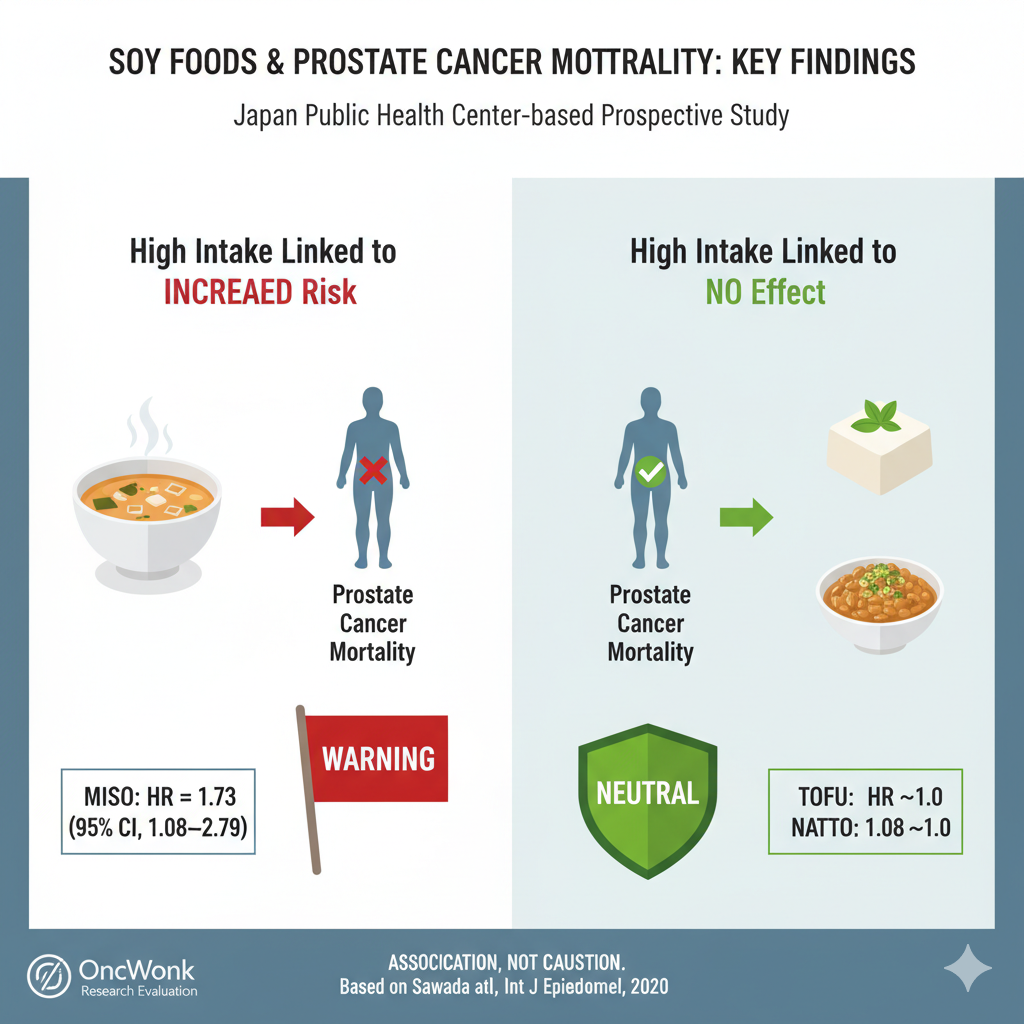
Not All Soy is Equal: This is perhaps the most important detail. The negative association was driven almost entirely by miso. In contrast, intake of natto and tofu—two other major soy foods—showed no significant association with prostate cancer mortality. This strongly suggests that the observed harm is not from “soy” or “isoflavones” as a general category, but from a factor specific to miso (e.g., its high salt content, other compounds from fermentation) or a lifestyle pattern associated with high miso consumption that wasn’t fully adjusted for.
-
Key Limitations: The study’s limitations are significant. Measuring diet only once at the beginning of a 17-year follow-up is a major weakness, as dietary habits can change dramatically over time. The lack of specific data on PSA screening and cancer treatment is also a critical gap.
This study effectively highlights a potential, specific risk for a subgroup of patients (perhaps those with advanced disease or on ADT) and a specific food (miso), while simultaneously undermining the idea that “soy” as a single category is the problem.
Summary:
Clinical Bottom Line
This large, prospective Japanese cohort study did not find a survival benefit associated with high soy or isoflavone consumption. On the contrary, it reports a statistically significant association between the highest intake of soy foods and an increased risk of prostate cancer mortality. This finding challenges previous research that suggested a protective effect. The authors speculate this discrepancy may be due to isoflavones having different effects based on cancer stage, potentially preventing localized cancer but adversely affecting advanced, lethal cancer. As an observational study, this finding shows an association, not causation, and highlights the need for further research into the complex role of soy in prostate cancer progression.
Results in Context
Main Results: Over an average follow-up of 16.9 years, 221 prostate cancer deaths were recorded among 43,580 men.
Soy Food: After adjusting for multiple confounders, men in the highest quintile (Q5) of soy food intake had a 76% higher risk of prostate cancer mortality compared to those in the lowest quintile (Q1) (Multivariate Hazard Ratio [HR] = 1.76; 95% CI, 1.10–2.82; p for trend = 0.04).
Isoflavones: A similar association was seen for total isoflavone intake, with the highest quintile of intake associated with an increased risk (Multivariate HR = 1.39; 95% CI, 0.87–2.20; p for trend = 0.04).
Specific Foods: When analyzing specific soy foods, high intake of miso showed a positive association with prostate cancer mortality (Q5 vs. Q1 Multivariate HR = 1.73; 95% CI, 1.08–2.79). Intake of natto and tofu showed a null association.
Definitions: A Hazard Ratio (HR) compares the risk of an event (in this case, death from prostate cancer) in one group versus another over time. An HR of 1.76 means the risk of the event is 76% higher in the high-intake group compared to the low-intake group, after accounting for other factors. The ‘p for trend’ value assesses whether the risk consistently increases (or decreases) across all quintiles of intake.
Participants: The analysis included 43,580 Japanese men aged 45-74 years who had no self-reported prior history of cancer or cardiovascular disease at the study’s starting point. Participants who reported extreme total energy intake were also excluded.
The Discrepancy in Findings
The central issue is that while overall soy food intake was linked to an increased risk of prostate cancer mortality, this association was not consistent across all soy products. The negative association appeared to be driven primarily by miso.
-
Overall Soy Food: The study found a positive association between high intake of total soy food and an increased risk of prostate cancer mortality (Multivariate Hazard Ratio [HR] = 1.76).
-
Miso: High intake of miso also showed a similar positive association with prostate cancer mortality (Multivariate HR = 1.73).
-
Natto and Tofu: In contrast, high intake of natto and tofu showed a null association, meaning no statistically significant link to prostate cancer mortality was found.
Authors’ Explanation for the Discrepancy
The authors state that the reason for this difference is “not clear”. However, they propose a hypothesis:
The difference might be due to other components in the foods, not just the isoflavones. They note that natto has a higher fiber and protein content per gram compared to miso. The authors speculate that this higher fiber and protein intake “may overcome the adverse effects of isoflavone intake on the progression of prostate cancer”.
They also acknowledge that the discrepancy could be due to “residual confounding,” meaning other unmeasured factors could be influencing the results.
Assertive Critical Appraisal
Limitations & Bias (STROBE Framework):
-
Confounding: As with all observational studies, unmeasured confounding variables could be influencing the results. The authors adjusted for a wide range of factors (e.g., age, study area, smoking, alcohol, BMI, physical activity, diabetes history, screening history, and intake of green tea, coffee, vegetables, and fruit), but residual confounding is always possible.
-
Misclassification: Dietary intake was measured only once at the study’s starting point using a food frequency questionnaire (FFQ). While the FFQ had been validated and showed good reproducibility, this single time-point measurement could lead to misclassification of intake if participants’ diets changed substantially over the average 17-year follow-up.
-
Missing Data: The study did not have information on treatment for prostate cancer or PSA screening for all subjects. The authors used “history of screening” (for any condition, such as blood pressure or chest X-ray) as a surrogate marker for health-seeking behavior, which is a significant limitation. They also lacked family history of prostate cancer at the starting point, though adjusting for this data collected 5 years prior did not change the results.
Reporting Quality Assessment (STROBE): The study’s reporting is strong. The authors clearly describe their efforts to address confounding by listing the variables included in their multivariate models. They explicitly state the potential for residual confounding as a limitation. The participant selection process is clearly detailed in a flow chart (Figure 1), and the methods for ascertaining the outcome (prostate cancer death via national Vital Statistics registries) are robust.
Context of Progression (Authors’ Hypothesis): The authors directly address the conflict with prior research. They cite their own previous studies from this same cohort, which suggested that isoflavones had preventive effects only on localized cancer but were associated with an increased risk of advanced prostate cancer. They propose two key mechanisms to explain this study’s mortality findings:
-
Receptor Expression: Advanced and lethal prostate cancers often have decreased expression of estrogen receptor beta (ER-$\beta$). Since isoflavones are thought to exert protective effects by binding to ER-$\beta$, this protective mechanism may be lost in advanced, lethal disease.
-
Biphasic Effects: Isoflavones might have biphasic (opposing) effects depending on the body’s hormonal environment. An animal study suggested genistein (an isoflavone) could be anti-androgenic in intact mice but show androgen agonistic activity in castrated mice. The authors hypothesize that in patients receiving hormone therapy (like anti-androgens), isoflavones might paradoxically promote cancer progression. Given that a high percentage of Japanese patients with prostate cancer receive androgen deprivation therapy (ADT), this is a plausible, though unproven, hypothesis.
Applicability
The findings are from a Japanese population, which has a traditionally high soy intake compared to Western populations. This makes the results highly relevant for this specific population but may limit generalizability to populations with different dietary habits, genetic backgrounds, and gut microbiomes (which affects isfoflavone metabolism). The findings specifically relate to prostate cancer mortality and progression, and the authors caution that the role of soy may be different for the prevention of localized disease.
Research Objective
To investigate the association between the intake of soy, soy products, and isoflavones and the subsequent risk of prostate cancer mortality in a large prospective study of Japanese men.
Study Design
Design: This was a population-based prospective cohort study (the Japan Public Health Center-based Prospective Study or JPHC Study).
Setting and Participants: The study enrolled men from 11 public health center areas in Japan. The final analysis cohort consisted of 43,580 men aged 45-74 who returned a 5-year follow-up questionnaire (which served as the study’s starting point) and had no self-reported history of cancer or cardiovascular disease.
Assessment: Dietary intake was assessed at the starting point using a validated 138-item food frequency questionnaire (FFQ).
Follow-up: Participants were followed from 1995 until 2016. Deaths from prostate cancer were classified using ICD-10 codes (C61) from the national Vital Statistics registry.
Bibliographic Data
Title: Soy and isoflavone consumption and subsequent risk of prostate cancer mortality: the Japan Public Health Center-based Prospective Study
Authors: Norie Sawada, Motoki Iwasaki, Taiki Yamaji, Taichi Shimazu, Manami Inoue, and Shoichiro Tsugane; for the Japan PublicHealth Center-based Prospective Study Group
Journal: International Journal of Epidemiology
Year: 2020
DOI: 10.1093/ije/dyaa177
This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
Full text: Article here.
