☢️Synthesized Clinical Bottom Line
Updated 11-16-2025
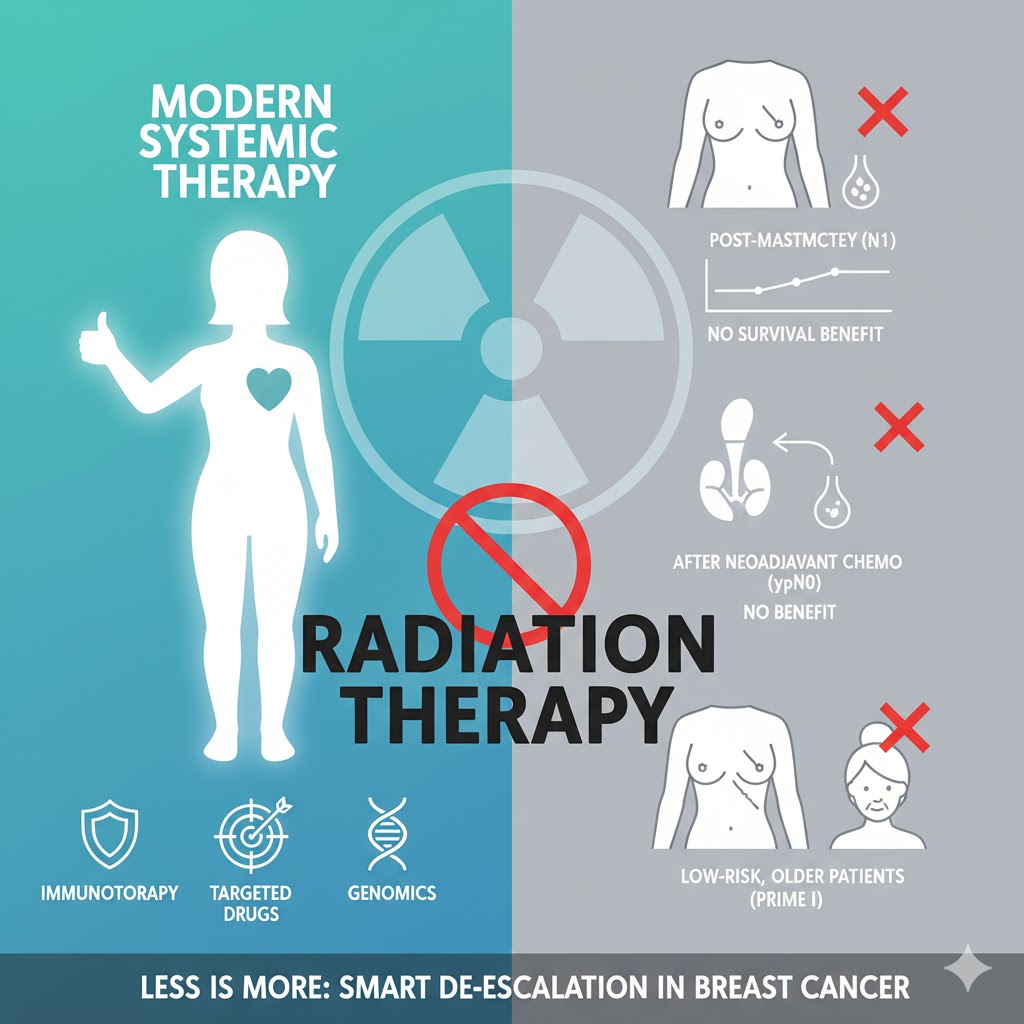
The provided collection of research, which includes three major Phase 3 randomized controlled trials (RCTs), supplies strong evidence for the de-escalation of radiation therapy in several common breast cancer settings. The central, unifying theme is that the survival benefits historically attributed to radiation have been substantially or entirely negated by the effectiveness of modern systemic therapies.
Key findings supporting this conclusion are:
-
Post-Mastectomy (Intermediate-Risk): For “intermediate-risk” patients (including T1-2N1) treated with mastectomy and contemporary systemic therapy, the SUPREMO trial (Kunkler et al., 2025) found no improvement in 10-year overall survival, disease-free survival, or distant metastasis-free survival with the addition of chest-wall radiation.
-
After Neoadjuvant Chemotherapy: For patients who are initially node-positive but achieve a complete pathological nodal response (ypN0) after neoadjuvant chemotherapy, the NSABP B-51 trial (Mamounas et al., 2025) found that adding regional nodal radiation provides no significant benefit to recurrence-free intervals or overall survival.
-
After Lumpectomy (Low-Risk, Older Patients): For older (≥65), low-risk (HR-positive, node-negative) patients, the PRIME II trial (Kunkler et al., 2023) demonstrated that omitting whole-breast radiation has no detrimental effect on 10-year overall survival, breast cancer-specific survival, or distant recurrence, though it does increase the risk of local recurrence.
Thematic Evidence Analysis
This synthesis is organized by clinical scenario to highlight where the evidence supports omitting radiation without compromising survival.
1. No Survival Benefit from Post-Mastectomy Radiation (PMRT) in Intermediate-Risk (N1) Disease
The most significant finding comes from the recent SUPREMO trial (Kunkler et al., 2025), which was designed to resolve the long-standing controversy over PMRT in “intermediate-risk” patients, a group that includes those with one to three positive lymph nodes (T1-2N1).
-
Primary Endpoint (Overall Survival): The trial randomized 1,607 patients to receive modern systemic therapy with or without chest-wall irradiation (CWI) after mastectomy. After a median follow-up of 9.6 years, the primary endpoint was not met. There was no difference in 10-year overall survival between the two groups (81.4% with CWI vs. 81.9% without CWI; P=0.80).
-
Secondary Endpoints (Recurrence and Survival): This lack of benefit extended to all key secondary survival endpoints. There was no significant difference in 10-year disease-free survival (76.2% vs. 75.5%) or distant metastasis-free survival (78.2% vs. 79.2%). The lack of overall survival benefit held true for the specific pN1 (one to three positive nodes) subgroup.
-
Context and Conflict Resolution: This high-quality RCT finding explains the conflict present in the other provided literature:
-
Explaining Older Trials: A Cochrane systematic review (Verma et al., 2023) did find that PMRT improved overall survival (HR 0.76). However, the review’s authors caution that this finding is based on a single study from an older era (DBCG 82 b&c) that used “suboptimal” systemic treatments and outdated radiotherapy techniques. The SUPREMO authors directly state that their trial’s negative result is likely because “higher breast cancer survival, owing to advances in… systemic therapy” has negated the benefit seen in those older trials.
-
Explaining Observational Data: The finding also helps resolve a conflict between two large observational SEER database studies. While one study (Yang et al., 2021) suggested a survival benefit for PMRT, another, more stringently matched (propensity score matching) SEER study (Li et al., 2020) found that PMRT was not correlated with better breast cancer-specific survival in T1-2N1 patients (HR 1.129; P=0.137). The definitive results from the SUPREMO RCT strongly support the conclusion from Li et al. that PMRT provides no survival benefit in this population when treated with modern systemic therapy.
-
2. No Benefit from Regional Nodal Radiation (RNI) after Neoadjuvant Chemotherapy (NAC) Response
The NSABP B-51/RTOG 1304 trial (Mamounas et al., 2025) provides clear evidence for de-escalating radiation in a specific population: patients who respond well to NAC. The trial studied patients who were clinically node-positive (cN1) at diagnosis but converted to pathologically node-negative (ypN0) after completing NAC.
-
Primary Endpoint (Recurrence-Free Interval): The trial found that adding RNI did not significantly improve the primary endpoint of invasive breast cancer recurrence-free interval (a composite of locoregional recurrence, distant recurrence, or death from breast cancer). The 5-year estimate was 92.7% with RNI versus 91.8% without RNI (P=0.51).
-
Secondary Endpoints (Survival): The addition of RNI also failed to show a benefit in any of the key secondary endpoints, including locoregional recurrence-free interval, distant recurrence-free interval, or overall survival.
This trial concludes that a good pathological response to modern systemic therapy successfully identifies a group of patients who can be spared regional nodal radiation without compromising their outcomes.
3. No Survival Benefit from Radiation after Lumpectomy in Low-Risk, Older Patients
The PRIME II trial (Kunkler et al., 2023) provides evidence for omitting radiation in a low-risk population undergoing breast-conserving surgery (BCS). The trial enrolled women aged 65 or older with HR-positive, node-negative, T1-2 (≤3 cm) breast cancer who all received adjuvant endocrine therapy.
-
Survival and Distant Recurrence Endpoints: While omitting radiation did result in a higher 10-year rate of local recurrence (9.5% vs. 0.9%), it had no detrimental effect on 10-year overall survival (80.8% in the no-radiation group vs. 80.7% in the radiation group).
-
Furthermore, omitting radiation did not negatively impact 10-year distant recurrence as the first event (1.6% vs. 3.0%) or breast cancer-specific survival (97.4% vs. 97.9%).
This trial demonstrates that for this specific low-risk, older population, omitting radiation is a safe option in terms of survival, allowing for a personalized discussion that balances the accepted risk of higher local recurrence against the avoidance of radiation’s side effects.
Overall Assessment of the Evidence
The collective evidence from these papers builds a robust and consistent narrative. They demonstrate that in the era of modern, effective systemic therapy, the role of radiation in improving survival has diminished significantly.
The data strongly support that radiation can be safely omitted without compromising distant recurrence rates or overall survival in specific, well-defined populations:
-
Intermediate-risk (N1) patients after mastectomy.
-
Clinically node-positive patients who achieve a complete nodal response (ypN0) to neoadjuvant chemotherapy.
-
Older, low-risk (N0, HR+) patients after breast-conserving surgery.
The primary conflict in the provided literature—namely, older meta-analyses and conflicting observational studies suggesting a survival benefit for PMRT in N1 disease—is effectively resolved by the recent, high-quality SUPREMO trial. This trial confirms that the historical benefit is no longer apparent, likely because modern systemic therapy is so effective at controlling micrometastatic disease.
List of Analyzed Papers
-
Kunkler et al. (2023): Breast-Conserving Surgery with or without Irradiation in Early Breast Cancer. N Engl J Med.
-
Mamounas et al. (2025): Omitting Regional Nodal Irradiation in Responders to Neoadjuvant Chemotherapy. N Engl J Med.
-
Verma et al. (2023): Post-mastectomy radiotherapy for women with early breast cancer and one to three positive lymph nodes. Cochrane Database of Systematic Reviews.
-
Yang et al. (2021): Postmastectomy radiation therapy can improve survival for breast cancer patients with 1-3 positive axillary lymph nodes: a retrospective cohort study using the SEER database. Translational Cancer Research.
-
Li et al. (2020): Real-world impact of postmastectomy radiotherapy in T1–2 breast cancer with one to three positive lymph nodes. Annals of Translational Medicine.
-
Kunkler et al. (2025): Ten-Year Survival after Postmastectomy Chest-Wall Irradiation in Breast Cancer. N Engl J Med.
This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
