Relative vs. Absolute Risk Reduction: Understanding the True Benefit of a Medical Study
When reviewing a new medical study—whether it involves a conventional drug, a supplement, or a lifestyle change—you will often see two different numbers used to describe the treatment’s effectiveness: the Relative Risk Reduction and the Absolute Risk Reduction.
These two terms can present dramatically different pictures of the same treatment, and understanding the difference is essential for determining how much a therapy truly benefits a patient.
1. The Power of Proportion: Relative Risk Reduction (RRR)
The Relative Risk Reduction (RRR) is the percentage used to describe how much a treatment reduces the original risk of an event (like a cancer recurrence) in a group of patients. It tells you the proportion of risk that was eliminated.
The RRR is a powerful statistical tool because it often generates a large, attention-grabbing percentage.
-
How to interpret RRR: This number is calculated by comparing the drop in risk only against the baseline risk in the untreated group. It can feel misleading because it doesn’t account for how common the event was in the first place.
Why RRR can sound exaggerated: Imagine a rare cancer that affects 10 people in a group of 1,000. If a new therapy cuts that risk in half, it prevents 5 cases. Because the risk was cut by 50% relative to the original risk, the RRR is 50%. This number sounds huge, but it doesn’t convey the small number of people actually helped.
2. The True Impact: Absolute Risk Reduction (ARR)
The Absolute Risk Reduction (ARR) is the real, tangible difference in the number of unfavorable outcomes between the treated group and the untreated group. It tells you the percentage of all people treated who were genuinely helped by the intervention.
-
How to interpret ARR: This is the most honest measure of benefit. If a study reports an ARR of 2%, it means that out of every 100 people treated, 2 people benefited from the treatment by avoiding the negative outcome.
The ARR is typically a much smaller, yet more accurate, percentage than the RRR. It’s the number that helps doctors and patients truly weigh the pros and cons of adopting a new therapy.
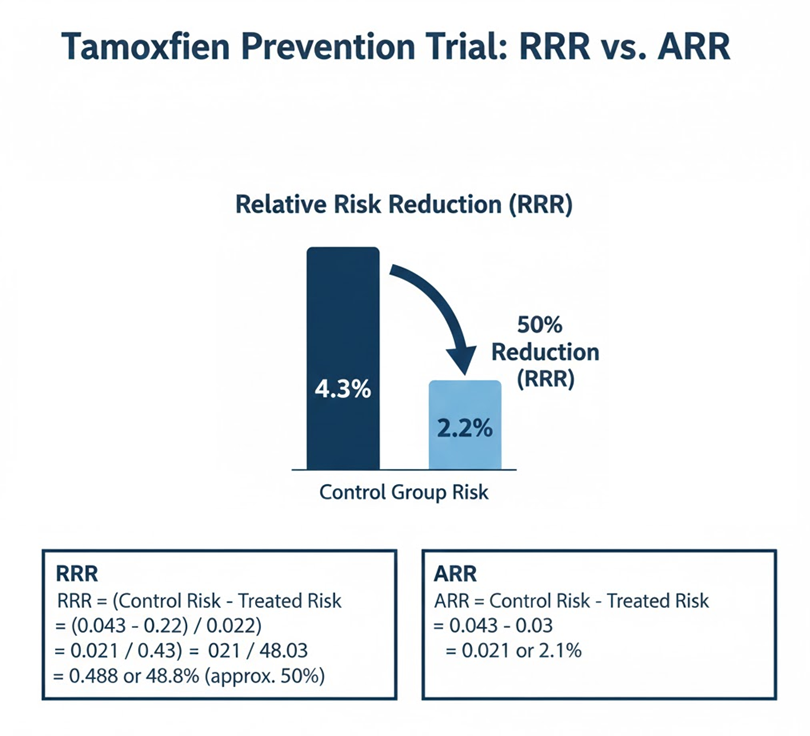
Case Study: Tamoxifen Prevention Trial (NSABP P-1)
A classic example of the difference between these two metrics comes from the National Surgical Adjuvant Breast and Bowel Project Breast Cancer Prevention Trial (NSABP P-1). This large study looked at whether the drug tamoxifen could prevent breast cancer in women who were considered high-risk.
When the results were reported, they provided a dramatic illustration of how Relative Risk Reduction can look huge while the Absolute Risk Reduction remains small.
| Outcome Measure | The Number Reported | What the Number Actually Means |
| Relative Risk Reduction (RRR) |
49% |
Tamoxifen reduced the proportional risk of developing invasive breast cancer by nearly half compared to women who received a placebo. |
| Absolute Risk Reduction (ARR) |
2.1% |
Over approximately six years, the actual number of women who avoided invasive breast cancer due to taking tamoxifen was only 2.1% of the total high-risk group. |
The Critical Difference
Why the huge difference? The 49% RRR comes from a high-risk group where the overall chance of developing invasive breast cancer (the baseline risk) was low—about 4.3% over the study period.
-
If the risk starts at 4.3% and you cut that risk by 49%, the new risk is about 2.2%.
-
The actual difference between 4.3% and 2.2% is just 2.1%.
In this scenario, the large RRR (49%) accurately describes the drug’s proportional potency (its ability to cut the risk), but the small ARR (2.1%) describes the true clinical magnitude (the number of people who were saved from developing the disease). For the individual patient, the ARR is the percentage that truly matters.
Summary: When evaluating research, always look beyond the large, impressive Relative Risk Reduction (RRR). Demand to know the Absolute Risk Reduction (ARR), as this number reveals the true percentage of people who benefited from the therapy and provides the most objective foundation for clinical decisions.
