Comment:
For years, people have been inappropriately scared of soy both in terms of causing breast cancer and negatively impacting progression once they have it. There is a group of people out there who are continuing to promote that despite all evidence to the contrary.
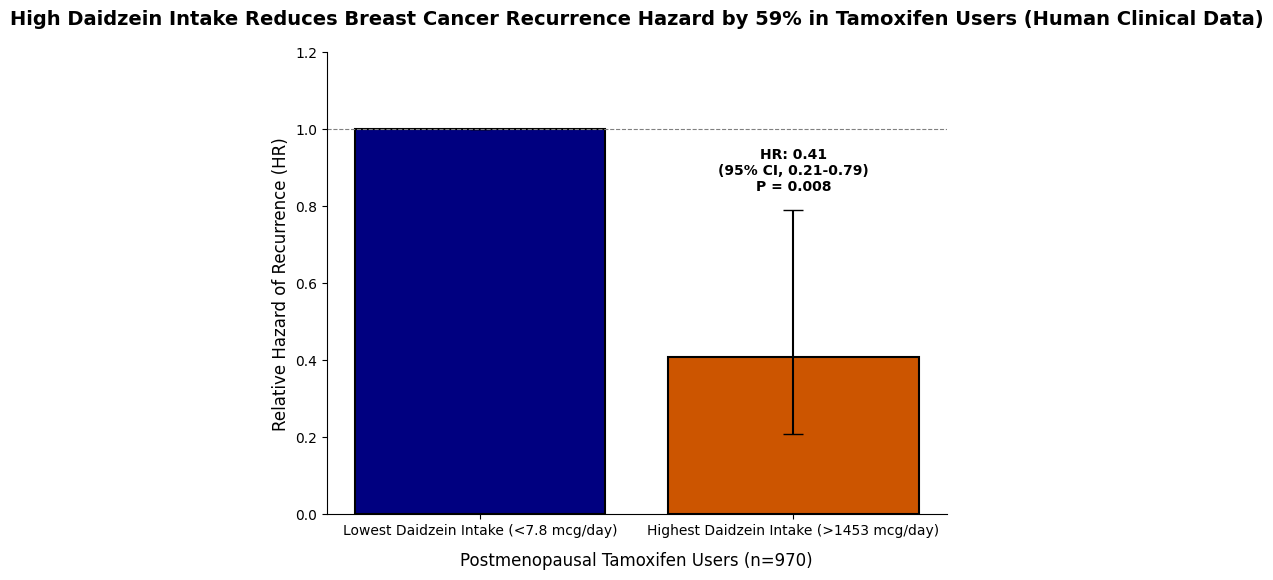
The key finding of this study is not just that soy appears safe, but that it may be actively beneficial in the specific group of postmenopausal women on tamoxifen. A ~60% reduction in recurrence is a striking signal, suggesting a potential synergistic interaction.
Summary:
Clinical Bottom Line
This prospective observational study of 1,954 breast cancer survivors suggests a potential beneficial association between high soy isoflavone intake and reduced cancer recurrence, but this benefit appears limited to specific patient subgroups. The strongest finding was an approximately 60% reduction in breast cancer recurrence for postmenopausal women using tamoxifen who had the highest daidzein intake (1453 mcg/day) compared to those with the lowest (7.8 mcg/day). The authors conclude that soy consumed at levels comparable to those in Asian populations may reduce recurrence risk in women receiving tamoxifen and, importantly, does not appear to interfere with tamoxifen’s efficacy.
However, as this is an observational study, these findings only demonstrate an association and cannot prove causation. The authors appropriately caution that these results require confirmation in other large studies before any clinical recommendations regarding soy intake can be issued to survivors.
Results in Context
Main Results
Overall Cohort (n=1954): In the full cohort, there was only a non-significant trend toward a decreasing risk of breast cancer recurrence with increasing intakes of daidzein (P=.20 for trend) and glycetin (P=.10 for trend).
Benefits in Subgroups: The potential benefits were most apparent when analyzing specific subgroups:
-
Postmenopausal Women: Suggestive trends for a reduced risk of recurrence were seen with increasing quintiles of daidzein (P=.08 for trend) and glycetin (P=.06 for trend) intake compared to no intake.
-
Tamoxifen Users: Among women who had ever used tamoxifen, there was a significant decreased risk of recurrence with increasing glycetin intake (P=.05 for trend) and suggestive trends for daidzein (P=.10) and genistein (P=.13).
-
Hormone Receptor-Positive Tumors: A decreasing risk of recurrence was observed with increasing isoflavone intake among women with tumors that were ER+ or PR+, but not among those with ER- and PR- tumors.
Key Finding (Postmenopausal Tamoxifen Users): The most statistically significant benefit was found in postmenopausal women treated with tamoxifen (n=970). In this group, women with the highest daidzein intake (>1453 mcg/day) had a 59% reduction in the hazard of recurrence compared to those with the lowest intake (<7.8 mcg/day) (HR, 0.41; 95% CI, 0.21-0.79, P=.008).
Definitions
The study used hazard ratios (HRs) to estimate risk. A hazard ratio below 1.0 indicates a reduced risk (a potential benefit) for the exposure group compared to the reference group. For example, the HR of 0.41 in the key subgroup means that women with the highest daidzein intake had a 59% lower rate of recurrence at any given time point compared to women with the lowest intake.
Participants
The analysis included 1,954 female breast cancer survivors from the Life After Cancer Epidemiology (LACE) Study.
-
Women were enrolled an average of 1.88 years after their initial diagnosis.
-
The cohort was followed for an average of 6.31 years after enrollment.
-
During the follow-up period, 282 breast cancer recurrences were confirmed.
Assertive Critical Appraisal
Limitations & Bias (STROBE Framework)
-
Observational Design: This study’s primary limitation is its observational design, which is susceptible to confounding. The authors acknowledge that the benefit seen in high soy consumers might be due to other unmeasured factors associated with high soy intake, such as an overall healthier lifestyle.
-
Multiple Comparisons: The analysis involved multiple subgroup tests (e.g., by menopausal status, tamoxifen use, hormone receptor status) and multiple isoflavones (daidzein, genistein, glycetin). The authors note they did not adjust for these multiple comparisons, which increases the risk of a Type 1 error (i.e., finding a statistically significant benefit by chance).
-
Low Soy Intake Population: The cohort was largely comprised of Caucasian females with generally low soy consumption. The average isoflavone intake was much lower than that reported in Asian populations. While the strongest protective effects were seen at the highest intake levels in this cohort, those levels were only comparable to the lowest levels of intake in Asian studies.
-
Dietary Assessment: Soy intake was assessed via food frequency questionnaires (FFQs) mailed to participants, on average, 23 months post-diagnosis. This method is subject to recall bias, and intake was only measured at one time point.
-
Generalizability: The findings cannot be generalized to women with advanced-stage breast cancer.
Reporting Quality Assessment (STROBE)
The authors clearly described their methods for addressing potential confounding variables. Covariates for the final statistical models were selected based on literature review, correlation analysis, and stepwise regression. The final adjusted models included numerous key variables, such as BMI, menopausal status, tumor stage, ER/PR status, age, race, and total energy intake.
Applicability
The study’s findings are most relevant to postmenopausal breast cancer survivors with hormone receptor-positive tumors who are being treated with tamoxifen. The results provide preliminary evidence that, in this specific group, soy intake may be beneficial and does not appear to negate the effects of tamoxifen. However, the authors strongly state that these results must be replicated before any practical guidelines on soy consumption can be issued to survivors.
Research Objective
The study’s purpose was to examine the association between soy isoflavone intake (daidzein, genistein, and glycetin) and the risk of breast cancer recurrence in a cohort of breast cancer survivors. It specifically aimed to evaluate this relationship stratified by menopausal status, hormone receptor status, and tamoxifen therapy.
Study Design
-
This was a prospective cohort study using data from the Life After Cancer Epidemiology (LACE) Study.
-
A cohort of 1,954 survivors was followed prospectively for an average of 6.31 years.
-
Dietary intake, including soy isoflavones, was assessed at baseline (on average 23 months post-diagnosis) using modified Block and supplemental soy food frequency questionnaires.
-
The primary endpoint was breast cancer recurrence, defined as local, regional, or distant recurrence, as well as new contralateral breast cancers.
-
Recurrences were ascertained through mailed questionnaires and verified by medical record review.
-
The statistical analysis used multivariable delayed-entry Cox proportional hazards models to estimate hazard ratios (HRs) and 95% confidence intervals (CIs).
Setting and Participants
-
Participants were 1,954 female breast cancer survivors recruited from the Kaiser Permanente Northern California Cancer Registry (82%), the Utah Cancer Registry (12%), and the WHEL Trial (6%).
-
Eligible women were diagnosed with primary breast cancer (Stage I > 1 cm, II, or IIIA) between 1997 and 2000.
-
Women had to be free of recurrence at enrollment and have completed primary cancer treatment (aside from adjuvant hormonal therapy).
Bibliographic Data
-
Title: Soy Isoflavones and Risk of Cancer Recurrence in a Cohort of Breast Cancer Survivors: Life After Cancer Epidemiology (LACE) Study.
-
Authors: Neela Guha, MPH; Marilyn L. Kwan, PhD; Charles P. Quesenberry Jr., PhD; Erin K. Weltzien, BA; Adrienne L. Castillo, MS; and Bette J. Caan, DrPH.
-
Journal: Breast Cancer Research and Treatment.
-
Year: 2009.
-
DOI: 10.1007/s10549-009-0321-5.
Mandatory Disclaimer: This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
Full text pdf: PubMed Central
