📝 Comment:
This trial provides a critical, high-level confirmation: modern systemic therapy has fundamentally changed the risk/benefit profile of post-mastectomy chest-wall irradiation (CWI) for intermediate-risk breast cancer.
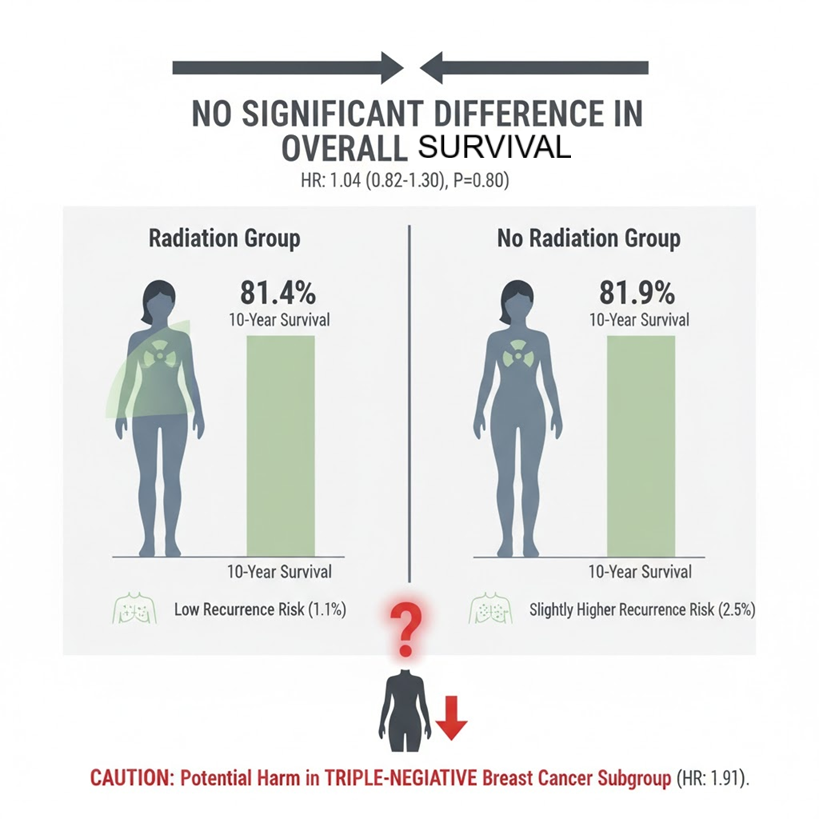
The key takeaway is that for the overall population, a minimal absolute reduction in local recurrence (less than 2 percentage points) did not translate into an Overall Survival (OS) benefit at 10 years. Simply put, we are failing to move the OS needle while still exposing patients to long-term cardiac and pulmonary toxicities. The data show an HR for death of 1.04 (P = 0.80), which is a clear failure to improve outcomes.
However, the most concerning, and potentially actionable, finding is the signal of significant harm in the TNBC subgroup, with a Hazard Ratio for death of 1.91 (95% CI, 1.06 to 3.46) with CWI. Given the consistency with data from the NSABP B-51/RTOG-1304 trial, this is something we must educate patients about unless this potential for immune-mediated detriment is definitively ruled out. This is a case of overtreatment potentially leading to worse survival.
Summary:
Clinical Bottom Line
This large, contemporary randomized controlled trial provides strong evidence that for patients with intermediate-risk, early breast cancer treated with mastectomy and modern systemic therapy, omitting chest-wall irradiation (CWI) does not compromise overall survival (OS) at 10 years . The 10-year OS was high in both the irradiation (81.4%) and no-irradiation (81.9%) groups . This suggests that modern systemic therapy has substantially reduced the risk of locoregional recurrence . The minimal absolute reduction in chest-wall recurrence (less than 2 percentage points) did not translate into an OS benefit .
However, the subgroup analysis suggested a potential negative effect of CWI for patients with triple-negative breast cancer (TNBC), who appeared to have lower overall survival with irradiation . This finding, while requiring further confirmation, is concerning and warrants caution in this specific patient population .
Results in Context
Primary Outcome
The primary end point was overall survival (OS), with 10 years of follow-up .
-
10-Year OS with CWI: 81.4% .
-
10-Year OS with No CWI: 81.9% .
-
Hazard Ratio (HR) for Death: 1.04 (95% confidence interval [CI], 0.82 to 1.30; P = 0.80) .
-
Interpretation: There was no significant between-group difference in overall survival, failing to show a benefit for CWI in the overall intermediate-risk population .
Key Secondary & Specialized Outcomes
-
Chest-Wall Recurrence: Occurred in 9 patients (1.1%) in the irradiation group and 20 patients (2.5%) in the no-irradiation group .
-
Finding: A reduction in risk was observed with irradiation (HR, 0.45; 95% CI, 0.20 to 0.99) .
-
Context: The absolute between-group difference was minimal (< 2 percentage points), suggesting contemporary systemic therapy effectively controls local disease, minimizing the benefit of added radiation .
-
Disease-Free Survival (DFS): 76.2% with CWI vs. 75.5% with no CWI (HR for recurrence or death, 0.97; 95% CI, 0.79 to 1.18) . No significant difference .
-
Distant Metastasis-Free Survival: 78.2% with CWI vs. 79.2% with no CWI (HR for distant metastasis or death, 1.06; 95% CI, 0.86 to 1.31) . No significant difference .
Harms and Adverse Events
-
Toxic effects of radiotherapy were generally mild .
-
The incidence of lung-related adverse events of grade 2 or higher was 2.59 times higher in the irradiation group (13 events vs. 5 events in the no-irradiation group) .
-
The incidence of heart-related and bone-related adverse events did not differ substantially .
-
Death from cardiac causes was low in both groups (0.7% in CWI vs. 1.0% in no CWI), though the authors note that radiation-induced cardiac disease can manifest more than 10 years after treatment .
Assertive Critical Appraisal
Risk of Bias (RoB 2 Framework): Low
The trial is judged to be at Low risk of bias. It was a phase 3, international, randomized trial . Randomization was stratified according to the treating center . The primary outcome, overall survival, is an objective, patient-important endpoint . The median follow-up of 9.6 years is sufficient to capture long-term OS data .
Subgroup Analyses: Potential Harm in TNBC
The subgroup analysis according to molecular subtype suggested a worse outcome with CWI for patients with triple-negative breast cancer (TNBC) .
-
Finding: The HR for death in the TNBC subgroup was 1.91 (95% \text{ CI}, 1.06 \text{ to } 3.46), suggesting a statistically significant increase in the hazard of death with irradiation .
-
Credibility Critique: While the effect is large and statistically significant, the claim must be treated with skepticism due to the small number of patients (31 deaths in 91 CWI patients vs. 17 deaths in 84 no-CWI patients) and events in this subgroup .
-
Contextual Relevance (Potential Harm): This finding is concerning because it is consistent with data from the NSABP B-51-RTOG-1304 trial . The authors speculate that this negative effect may be due to a detrimental effect of radiation on immune modulation, suggesting a biological plausibility for the finding . Clinicians should be highly cautious about recommending chest-wall irradiation for intermediate-risk TNBC patients until this is definitively ruled out in future studies .
Composite Endpoints
Secondary outcomes included composite endpoints like Disease-Free Survival and Distant Metastasis-Free Survival . Since the treatment effect was not consistent across individual components (the reduction in local recurrence was minimal and did not improve OS), and the composite outcomes were negative, this confirms the lack of overall clinical benefit .
Reporting Quality Assessment (CONSORT)
The reporting quality is high . A clear participant flow diagram (Figure 1) is included, and the methods for randomization (1:1 ratio, permuted blocks with varied block sizes) and stratification are adequately described .
Applicability
The findings are highly applicable to current general clinical practice . The eligibility criteria defining intermediate-risk (e.g., pN1 or pN0 with high-risk features like grade 3, LVI) reflect contemporary risk stratification . The near-universal use of modern systemic therapy (84.8% chemotherapy, 78.7% endocrine therapy, 19.8% trastuzumab) ensures the results are relevant to modern multidisciplinary management .
Research Objective & Design
Research Objective
To evaluate whether the omission of chest-wall irradiation leads to lower overall survival in women with intermediate-risk breast cancer (pT1N1, pT2N1, or pT3N0, or pT2N0 with grade 3, LVI, or both) who were treated with mastectomy, an axillary procedure, and systemic therapy .
Study Design
-
Design: International, phase 3, randomized clinical trial .
-
Allocation and Blinding: Patients were randomly assigned in a 1:1 ratio to undergo CWI or not to undergo CWI . The nature of the intervention prevents blinding .
-
Participants: A total of 1679 patients underwent randomization; 808 were included in the CWI group and 799 in the no-CWI group for the intention-to-treat analysis .
Setting and Participants
-
Setting: 125 sites in the United Kingdom, EORTC sites (7 countries in continental Europe, Israel, Turkey), and 21 other international sites .
-
Eligibility: Women undergoing mastectomy for intermediate-risk, stage II cancer without distant metastases . Intermediate-risk was defined based on tumor size and nodal status (pT1N1, pT2N1, or pT2N0 with grade 3 or lymphovascular invasion) .
Bibliographic Data
Title Ten-Year Survival after Postmastectomy Chest-Wall Irradiation in Breast Cancer
Authors I.H. Kunkler, N.S. Russell, N. Anderson, R. Sainsbury, J.M. Dixon, D. Cameron, et al. for the SUPREMO Trial Investigators
Journal The NEW ENGLAND JOURNAL of MEDICINE
Year 2025
DOI 10.1056/NEJMoa2412225
Mandatory Disclaimer: This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
Original Article: Ten-Year Survival after Postmatectomy Chest-Wall Irradiation in Breast Cancer
