📝 Comment:
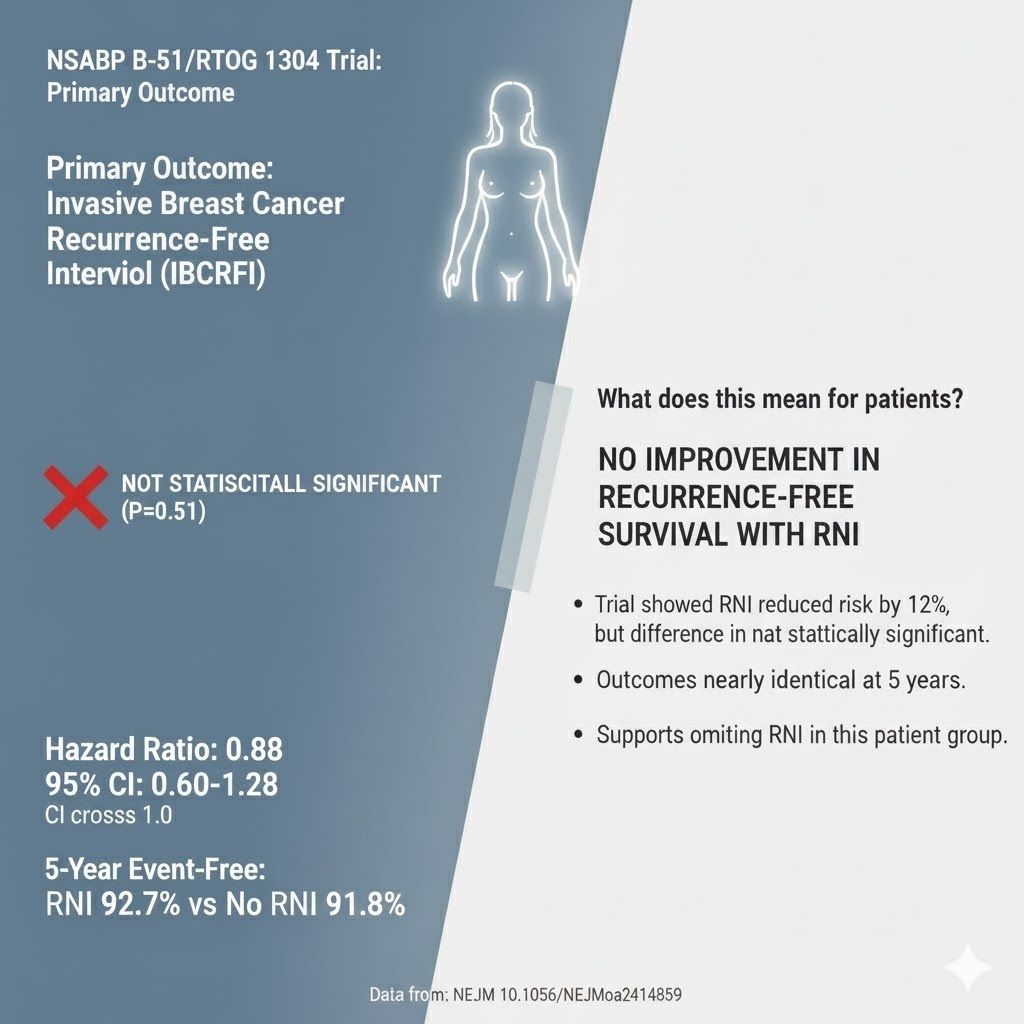
This trial delivers definitive knowledge: Regional Nodal Irradiation (RNI) offers no measurable oncologic benefit for the increasingly common patient population that achieves pathologic complete response (ypN0) after neoadjuvant chemotherapy.
The five-year data unequivocally demonstrate that RNI fails to significantly improve the primary endpoint—invasive breast cancer recurrence-free interval (HR 0.88, p = 0.51)—or any key secondary endpoint, including Overall Survival (OS). It provides the necessary prospective evidence to resolve prior uncertainty, allowing us to confidently omit RNI in these patients. This is a clear victory for de-escalation of locoregional therapy, as we can spare patients the higher rates of Grade 3 toxicity (10.0% vs. 6.5%)—particularly radiation dermatitis—without sacrificing oncologic control.
Summary:
🎯 Clinical Bottom Line
This definitive Phase 3 randomized controlled trial provides strong evidence that adding adjuvant regional nodal irradiation (RNI) offers no oncologic benefit in patients with clinically node-positive breast cancer whose axillary lymph nodes convert to pathologically negative (ypN0) after neoadjuvant chemotherapy. At a median follow-up of nearly five years, RNI did not significantly improve the primary endpoint—invasive breast cancer recurrence-free interval—nor any of the key secondary endpoints, including overall survival. This finding supports the de-escalation of locoregional therapy by omitting RNI in this specific, increasingly common patient population.
Results in Context
Primary Outcome: Invasive Breast Cancer Recurrence-Free Interval (IBCRFI)
The primary endpoint, defined as the time from randomization to invasive locoregional recurrence, distant recurrence, or death from breast cancer, was not significantly improved with the addition of RNI.
- Hazard Ratio (HR): 0.88.
- Definition: A hazard ratio of 0.88 means that the instantaneous risk (hazard) of having an IBCRFI event was 12% lower in the RNI group compared to the no-RNI group over the follow-up period, but this difference was not statistically significant.
- 95% Confidence Interval (CI): 0.60 to 1.28.
- Interpretation: Because the confidence interval crosses 1.0, the result is considered statistically non-significant (P = 0.51).
- 5-Year Estimate of Survival Free from Primary End-Point Events: 92.7% in the RNI group vs. 91.8% in the no-RNI group.
Key Secondary & Specialized Outcomes
RNI did not significantly improve any secondary outcomes at 5 years.
|
Outcome |
RNI Event Rate (5-yr Estimate) |
No RNI Event Rate (5-yr Estimate) |
Hazard Ratio (95% CI) |
Significance |
|
Locoregional Recurrence-Free Interval (LRRFI) |
6 events (98.9%) |
11 events (98.4%) |
0.57 (0.21, 1.54) |
No |
|
Distant Recurrence-Free Interval (DRFI) |
46 events (93.4%) |
48 events (93.4%) |
1.00 (0.67, 1.51) |
No |
|
Disease-Free Survival (DFS) |
85 events (88.3%) |
83 events (88.5%) |
1.06 (0.79, 1.44) |
No |
|
Overall Survival (OS) |
49 deaths (93.6%) |
45 deaths (94.0%) |
1.12 (0.75, 1.68) |
No |
Harms and Adverse Events
- No deaths related to the protocol-specified therapy were reported.
- No unexpected adverse events were observed.
- Grade 4 adverse events were rare: 0.5% in the irradiation group vs. 0.1% in the no-irradiation group.
- Grade 3 toxicity was uncommon but higher with RNI: 10.0% vs. 6.5%.
- The most common Grade 3 adverse event was radiation dermatitis, occurring in 5.7% of the RNI group and 3.3% of the no-RNI group.
Assertive Critical Appraisal
Risk of Bias (RoB 2 Framework)
- Overall RoB Judgment: Low
The NSABP B-51/RTOG 1304 trial is a high-quality, multicenter, randomized Phase 3 trial. The study design minimizes bias through:
- Randomization: Patients were randomly assigned to treatment arms after completing neoadjuvant chemotherapy and having confirmed ypN0 status, ensuring balance in known and unknown prognostic factors.
- Centralized Quality Assurance: A two-step radiation quality-assurance process and centralized benchmarking were required to ensure accurate delivery of radiation therapy, which rules out variation in treatment quality as an explanation for the lack of benefit.
- Potential Flaw (Low Event Rate): The observed primary end-point event rate (8.2%) was around one-third lower than projected. Consequently, the trial conducted a time-driven analysis with only 109 events, considerably less than the 172 events specified for the original event-driven final analysis. This under-accrual of events reduces the power of the study to detect a true difference, potentially leading to a Type II error (failing to detect a real treatment effect). Longer follow-up is necessary to provide more definitive long-term results.
Subgroup Analyses
Exploratory analyses hint at potential differences in effect based on tumor subtype:
- Triple-Negative Breast Cancer (TNBC): RNI had a numerically higher hazard for the primary event (HR 2.30; 95% CI, 1.00 to 5.25). The authors caution this is likely a spurious finding because most TNBC recurrences happen within five years, and the result is clinically counter-intuitive.
- Hormone Receptor-Positive/HER2-Negative: A trend toward RNI benefit was noted (HR 0.41; 95% CI, 0.17 to 0.99). The authors note that these patients generally have a longer time to recurrence, meaning additional follow-up is needed for a definitive assessment of RNI benefit in this subgroup.
Subgroup claims should be viewed with skepticism, as the number of patients in these subsets is small, resulting in wide confidence intervals, and the study was not powered for these comparisons.
Composite Endpoints
The Invasive Breast Cancer Recurrence-Free Interval (IBCRFI) is a composite endpoint.
- Components: Invasive locoregional recurrence, distant recurrence, or death from breast cancer.
- Clinical Importance: All components are clinically important, representing a failure of oncologic control.
- Consistency of Effect: The effect of RNI was not significant for any of the main endpoints (LRRFI, DRFI, OS), supporting the overall finding of no benefit for the composite endpoint.
Reporting Quality Assessment (CONSORT)
The abstract provides detailed results for the primary and secondary outcomes, including hazard ratios, confidence intervals, and P values. The number of patients at key stages of the analysis (enrolled, included in primary-event analysis) and the median follow-up are clearly reported. Although a formal CONSORT checklist is not in the provided text, the reporting quality is high, including reporting figures similar to the required flow diagram and detailed tables of events and subgroups.
Applicability
The findings are highly applicable to current general clinical practice. As neoadjuvant chemotherapy use increases, more patients who present with node-positive disease are achieving ypN0 status. This study provides the first prospective data to resolve clinical uncertainty, justifying the omission of RNI in this patient group, which can reduce the risk of radiation-related toxicity (e.g., Grade 3 dermatitis).
Research Objective and Study Design
Research Objective
The trial aimed to evaluate whether regional nodal irradiation would significantly improve the invasive breast cancer recurrence-free interval in patients with biopsy-proven, clinically node-positive breast cancer who achieve pathologically tumor-free (ypN0) status after neoadjuvant chemotherapy.
Study Design
- Design: Prospective, Phase 3, multicenter, randomized trial.
- Allocation: Patients were randomly assigned to receive regional nodal irradiation (RNI) or to omit RNI.
- Blinding: The blinding status is not explicitly stated in the provided text, but it is typically not feasible to blind for a radiation therapy intervention.
- Participants:
- Enrolled: 1,641 patients.
- Included in Primary-Event Analysis: 1,556 patients.
- Irradiation group: 772.
- No-irradiation group: 784.
Setting and Participants
- Setting: Multicenter trial conducted and overseen by NRG Oncology, a member of the National Clinical Trials Network.
- Eligibility Criteria: Patients with operable breast cancer (clinical stage T1-T3, N1, M0) confirmed to have axillary node involvement by biopsy before neoadjuvant chemotherapy. Crucially, they must have achieved pathologically tumor-free axillary nodes (ypN0) at surgery (lumpectomy or mastectomy) after neoadjuvant chemotherapy.
- Patient Characteristics (Balanced between groups): Median age was 52 years. The study population was enriched for high-risk subtypes: 57% HER2-positive and 21-23% triple-negative, with these two groups comprising 79% of the study population, reflecting the types of tumors most likely to achieve a pathologic complete response.
Bibliographic Data
- Title: Omitting Regional Nodal Irradiation in Responders to Neoadjuvant Chemotherapy
- Authors: Eleftherios P. Mamounas, M.D., Hanna Bandos, Ph.D, Julia R. White, M.D., et al.
- Journal: N Engl J Med
- Year: 2025 (Published in final edited form: June 05, 2025)
- DOI: 10.1056/NEJMoa2414859
Mandatory Disclaimer: This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Let me know if you would like me to draft a title or an introduction for the blog post based on this analysis.
Original Article:
Full text: Omitting Regional Nodal Irradiation after Response to Neoadjuvant Chemotherapy
