Comment:
This SEER data review of T1-2N1 breast cancer patients continues the trend we’ve been observing: Postmastectomy Radiotherapy (PMRT) rarely translates into a statistically significant survival advantage in the modern setting.
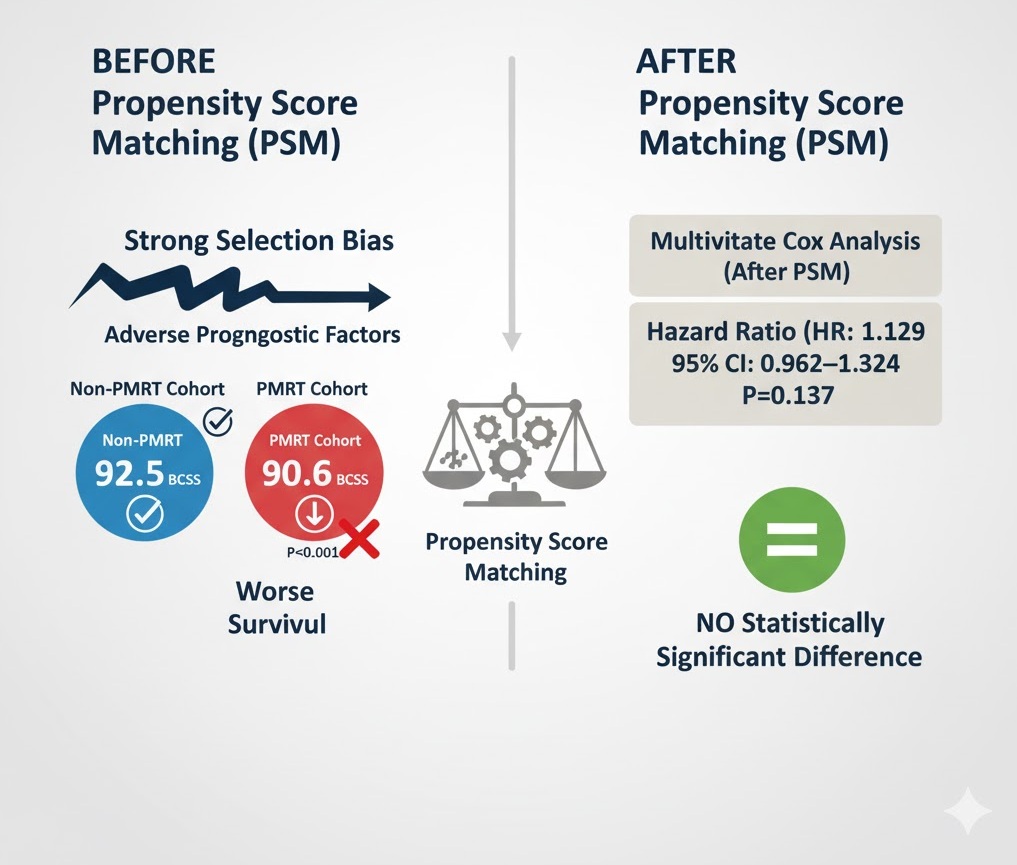
After adjusting for selection bias using Propensity Score Matching (PSM), the 5-year Breast Cancer-Specific Survival (BCSS) was comparable between the PMRT and non-PMRT groups. The raw data initially showed worse survival in the PMRT cohort, reinforcing that the patients selected for radiation already had more adverse prognostic factors. Of course, we would prefer to have Overall Survival data, which would be more likely to show any other negative consequences that aren’t capture by DSS.
This study adds yet more real-world evidence supporting a highly individualized approach. For the average T1-2N1 patient who receives adequate modern systemic therapy, the risk of Locoregional Recurrence (LRR) is already low (3.2–6.1%). Given that there is no absolute survival benefit, we must critically re-evaluate the risk-benefit profile of PMRT for this group, prioritizing patient quality of life and avoiding unnecessary adverse effects.
Summary:
Clinical Bottom Line
This large, real-world retrospective cohort study using SEER data suggests that postmastectomy radiotherapy (PMRT) does not provide a survival benefit for T1-2N1 breast cancer patients who have received modern systemic therapy and adequate axillary dissection. The 5-year breast cancer-specific survival (BCSS) was comparable between the PMRT and non-PMRT groups after accounting for confounding factors using propensity score matching (PSM). This finding supports a more selective approach to PMRT in this patient subset, especially given the potential for adverse effects.
Results in Context
Main Results
-
Disease Specific Survival (Before PSM): Before propensity score matching, the PMRT cohort actually showed a worse 5-year BCSS than the non-PMRT cohort (90.6% vs. 92.5%; log-rank test, P<0.001). This counterintuitive finding highlights the presence of strong selection bias, as patients with more adverse prognostic factors were more likely to receive PMRT.
-
Disease Specific Survival (After PSM): After using PSM to adjust for differences in patient and tumor characteristics, the receipt of PMRT was not correlated with better BCSS.
-
Multivariate Cox analysis after PSM yielded a Hazard Ratio (HR) of 1.129 (95% CI: 0.962–1.324; P=0.137), indicating no statistically significant difference in survival.
-
PMRT Utilization Trend: The use of PMRT significantly increased during the study period (2004–2012), rising from 30.6% in 2004 to 47.1% in 2012 (P<0.001). This increase, particularly after 2008, may be related to the publication of older trial data and changes in clinical guidelines.
-
Independent Predictors of PMRT Receipt: Factors independently associated with the administration of PMRT included:
-
Diagnosis after 2008.
-
Age <50 years.
-
Higher tumor grade (Poorly/undifferentiated, HR=1.745; Moderately differentiated, HR=1.409).
-
T2 tumor stage (HR=1.583).
-
≥ 2 positive lymph nodes (2 nodes, HR=1.497; 3 nodes, HR=2.640).
-
Definitions
-
Breast Cancer-Specific Survival (BCSS): Estimated from the time of breast cancer diagnosis to the time of death specifically from breast cancer or the follow-up cutoff.
-
Hazard Ratio (HR): A measure of how often an event (in this case, death from breast cancer) occurs in one group compared to another. An HR of 1.129 suggests a 12.9% increase in the hazard of breast cancer-specific death in the PMRT group, though the 95% Confidence Interval (0.962–1.324) crosses 1, meaning the finding is not statistically significant.
Assertive Critical Appraisal
Limitations & Bias (STROBE Framework)
-
Confounding is the Major Flaw (Selection Bias): This was a retrospective observational study, and the primary limitation is the inherent selection bias. The raw data showed the PMRT group had worse survival, which occurred because patients with more adverse prognostic factors (e.g., higher tumor grade, T2 stage, \ge 2 positive nodes) were the ones selected for PMRT. While the use of Propensity Score Matching (PSM) attempts to mitigate this by balancing known covariates, unmeasured confounding remains a serious threat. Factors such as systemic therapy details, HER2 status, and lymphovascular invasion (LVI)—which are all critical determinants of recurrence and survival—were not available in the SEER database and could not be adjusted for.
-
Uncertainty Regarding Systemic Therapy: The SEER database does not record the specifics of chemotherapy, endocrine therapy, or targeted therapy (such as Herceptin). The authors assumed modern systemic treatments were used, which is critical to their conclusion, but this cannot be confirmed. The effectiveness of modern systemic therapy in reducing locoregional recurrence (LRR) is the main rationale for questioning the need for PMRT. The lack of this data weakens the certainty of the conclusion.
-
Reporting Quality Assessment (STROBE): The paper provides a good description of the eligibility criteria and key variables, which aligns with STROBE guidelines. However, it explicitly states that crucial confounding variables (e.g., HER2 status, LVI, chemotherapy details) could not be addressed due to limitations in the SEER database. This is a major reporting flaw, as the authors cannot fully describe their efforts to adjust for the most critical sources of bias in this specific clinical question.
Applicability
The study’s applicability is high for general clinical practice in the modern era. It draws from a large, population-based US database (SEER) and focuses on the most common subgroup where PMRT utility is debated (T1-2N1). The findings suggest that clinicians should continue to individualize the decision for PMRT, considering that in the presence of modern systemic therapy, the survival benefit of PMRT for the average T1-2N1 patient may be negligible, but its adverse effects are real. The absolute risk of locoregional recurrence (LRR) in the modern era without PMRT is already low (3.2–6.1% at 5 years), meaning the absolute benefit is likely small.
Research Objective
The aim of this population-based study was to investigate the effectiveness of postmastectomy radiotherapy (PMRT) on breast cancer-specific survival (BCSS) in T1-2N1 breast cancer patients treated with mastectomy in the context of current clinical practice.
Study Design
-
Study Design: Retrospective cohort study using a population-based cancer registry database (Surveillance, Epidemiology, and End Results (SEER) program).
-
Key Methodology: Patients were divided into two cohorts: those who received PMRT and those who did not. The primary analysis used multivariate Cox proportional hazard survival analysis. To address selection bias, the researchers used 1:1 Propensity Score Matching (PSM), which matched patients in the PMRT and non-PMRT groups based on baseline characteristics such as age, tumor stage, grade, HoR status, and lymph node count.
Setting and Participants
-
Setting and Dates: Data was collected from the SEER program, a cancer statistics resource from 18 cancer registries in the United States. Data for patients diagnosed between 2004 and 2012 was included.
-
Participants: A total of 10,248 T1-2N1 breast cancer patients were included in the initial analysis.
-
Inclusion Criteria: Pathologically confirmed diagnosis of T1-2N1 invasive ductal carcinoma, treated with mastectomy and lymph node dissection (removal of \ge 10 lymph nodes), and received chemotherapy with or without PMRT.
-
Groups: 3,725 patients (36.3%) received PMRT, and 6,523 patients (63.7%) did not receive PMRT.
-
PSM Cohort: A total of 2,711 pairs of patients were matched for the propensity score analysis.
Bibliographic Data
-
Title: Real-world impact of postmastectomy radiotherapy in T1–2 breast cancer with one to three positive lymph nodes
-
Authors: Feng-Yan Li, Chen-Lu Lian, Jian Lei, Jun Wang, Li Hua, Zhen-Yu He, San-Gang Wu
-
Journal: Annals of Translational Medicine
-
Year: 2020
-
DOI: 10.21037/atm.2020.03.49
Mandatory Disclaimer: This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
