Comment:
Although this study came out almost 10 years ago, I still regularly have to reassure patients that it’s fine to take a blood pressure or do a blood draw or the side of their surgery. For decades, the caution against ipsilateral blood draws, BP checks, injections, and flying was “logical”—it made sense that trauma or compression could disrupt a compromised lymphatic system.
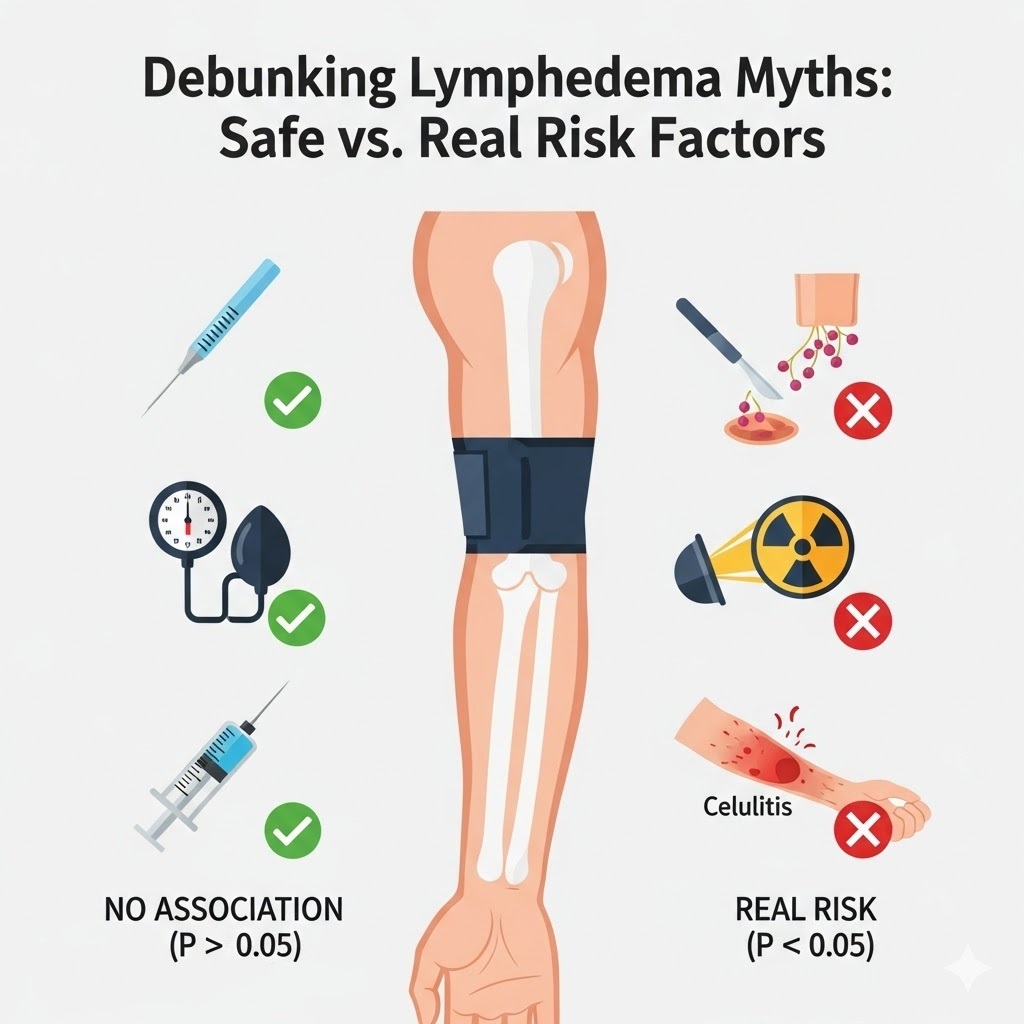
However, as this prospective cohort study clearly demonstrates, what sounds logical isn’t always correct when subjected to rigorous research. The data here show no significant association between these specific behaviors and an increased risk of lymphedema (BCRL).
Summary:
Clinical Bottom Line
This prospective cohort study challenges long-standing, anxiety-inducing precautionary guidelines by finding no significant association between ipsilateral blood draws, injections, blood pressure measurements, or air travel and an increased risk of breast cancer-related lymphedema (BCRL) . While these historically “taboo” behaviors appeared safe in this cohort, the study reaffirmed that established clinical factors—specifically high BMI, axillary lymph node dissection (ALND), regional lymph node radiation, and cellulitis—remain the strongest predictors of arm swelling . Clinicians may use these data to reassure patients and reduce the burden of lifelong behavioral restrictions, although caution regarding infection prevention (cellulitis) remains critical.
Results in Context
- Main Results (Non-Precautionary Behaviors): In a cohort of 632 patients undergoing 3,041 measurements, the study found no statistically significant association between increases in arm volume and the following patient-reported behaviors:
- Blood Draws: One or more ipsilateral draws vs. none (P = .62) .
- Injections: One or more ipsilateral injections vs. none (P = .77) .
- Air Travel: Number of flights (1-2 flights: P = .77; 3+ flights: P = .91) or duration of flights (P = .43) .
- Blood Pressure Measurements: While blood pressure readings showed a trend in univariate analysis (P = .034), this significance disappeared in the multivariate analysis, suggesting it was confounded by other factors .
- Main Results (Established Risk Factors): Multivariate analysis identified the following independent predictors of arm volume increase:
- Body Mass Index (BMI): BM I ≥ 25 was significantly associated with volume increase (P = .0236) .
- Axillary Surgery: Axillary Lymph Node Dissection (ALND) was a strong predictor (P < .001) .
- Radiation: Regional Lymph Node Irradiation (RLNR) (P = .0364) .
- Infection: Cellulitis was strongly associated with lymphedema risk (P < .001) .
Definitions & Participants
- Lymphedema Definition: Defined as a Relative Volume Change (RVC) or Weight-Adjusted Change (WAC) of ≥ 10% compared to baseline .
- Relative Volume Change (RVC): A formula comparing the surgical arm to the contralateral arm to account for non-treatment-related weight changes.
- Participants:
- The study included 632 patients with invasive breast cancer, contributing 3,041 postoperative measurements .
- Measurements were obtained using an optoelectric Perometer .
Assertive Critical Appraisal
- Limitations & Bias (STROBE Framework):
- Low Incidence of “Risk” Events: The study is limited by the low frequency of the behaviors being studied. Only 2.1% of responses reported injections and 8.5% reported blood draws . Critique: This low incidence significantly reduces the statistical power to detect a small adverse effect if one exists. The lack of an association might be due to a lack of “exposure” rather than proof of safety.
- Follow-Up Duration: The median follow-up was 24 months . While the average onset of lymphedema is 14.4 months , lymphedema can develop years later. A 2-year window may miss late-onset cases triggered by cumulative trauma.
- Recall Bias: Data on risk behaviors were collected via survey at the time of measurement . While prospective regarding the outcome, the exposure data relies on patient memory since the last visit (median 7 months) , introducing potential recall error.
- Confounding: The analysis did not adjust for the use of physical therapy . If patients who had minor trauma immediately sought PT, it could have masked the development of lymphedema.
- Reporting Quality Assessment (STROBE):
- Adjustment for Confounders: The authors appropriately utilized multivariate linear random effects models to adjust for known risk factors like BMI and type of surgery . This strengthens the validity of the null findings regarding blood draws and BP checks.
- Cellulitis Handling: The authors correctly excluded cellulitis from the model selection process to avoid overadjustment bias, as cellulitis lies on the causal pathway between trauma and lymphedema .
- Applicability:
- The findings are highly applicable to general breast cancer populations. The use of objective Perometer measurements rather than subjective tape measurements adds reliability to the findings .
- The results support the findings of the PAL trial, which also found no association between these behaviors and arm swelling .
Study Details
- Research Objective To investigate the association between blood draws, injections, blood pressure readings, trauma, cellulitis in the at-risk arm, and air travel on increases in arm volume in a cohort of patients treated for breast cancer .
- Study Design
- Design: Prospective cohort study .
- Methodology: Bilateral arm volume measurements were taken preoperatively and postoperatively at regular intervals (3-7 months) . At each visit, patients self-reported “risk events” occurring since the last measurement .
- Analysis: Linear random effects models were used to assess associations between events and relative arm volume changes .
- Setting and Participants
- Setting: Massachusetts General Hospital, United States .
- Study Period: 2005 to 2014 .
- Population: 632 patients with newly diagnosed invasive breast cancer screened for lymphedema .
- Key Exclusions: Patients were censored upon diagnosis of distant metastases, recurrence, or if they wore a compression sleeve while flying .
Bibliographic Data
- Title: Impact of Ipsilateral Blood Draws, Injections, Blood Pressure Measurements, and Air Travel on the Risk of Lymphedema for Patients Treated for Breast Cancer
- Authors: Ferguson CM, Swaroop MN, Horick N, Skolny MN, Miller CL, Jammallo LS, Brunelle C, O’Toole JA, Salama L, Specht MC, Taghian AG
- Journal: Journal of Clinical Oncology
- Year: 2016
- DOI: 10.1200/JCO.2015.61.5948
Original Article:
Full text html: here
