Comment:
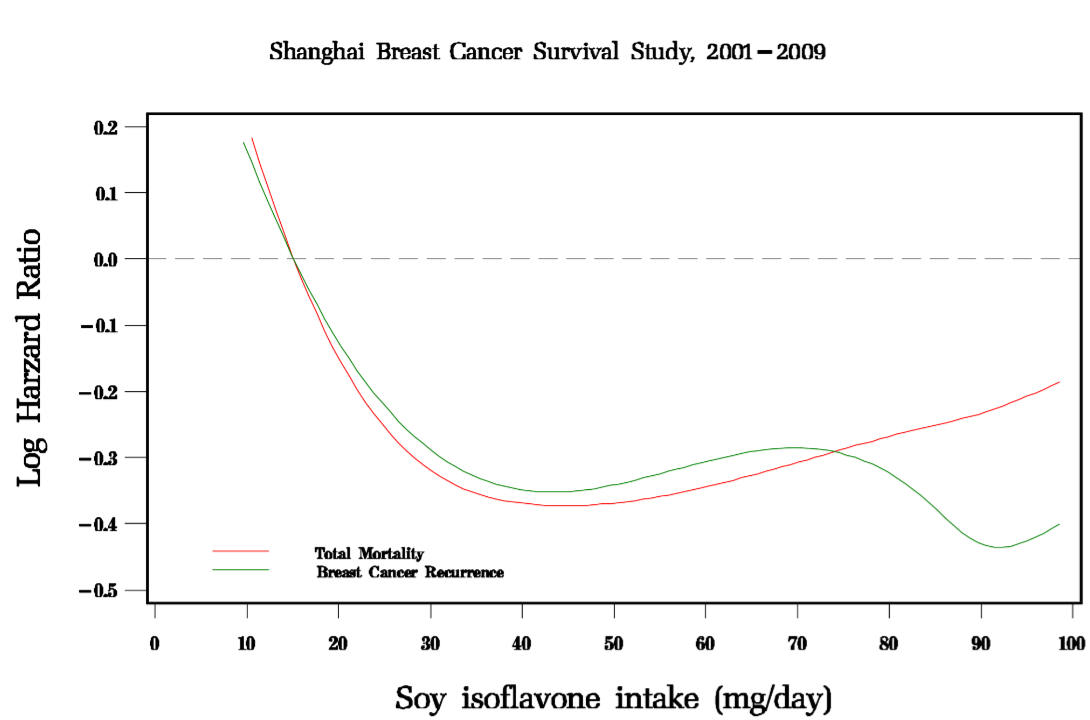
This study shows that in breast cancer patients, soy consumption was associated with reduced rates of both recurrence and death from breast cancer, as well as improved overall survival, not only breast cancer specific survival.
Summary:
Clinical Bottom Line:
This large, population-based cohort study of 5,033 Chinese breast cancer survivors found that higher soy food consumption after diagnosis was significantly associated with a decreased risk of both death and cancer recurrence. The beneficial association was observed in women with ER-positive and ER-negative cancers, as well as in both tamoxifen users and non-users. As an observational study, these findings show a strong association but cannot prove that soy consumption causes the improved outcomes; the results could be influenced by other unmeasured lifestyle factors.
Results in Context
Main Results:
The study followed participants for a median of 3.9 years. The analysis compared outcomes for women based on their level of soy protein intake, divided into four groups (quartiles).
-
Impact on Mortality: Women in the highest intake quartile had a 33% lower hazard of death from any cause compared to women in the lowest intake quartile (Hazard Ratio [HR] = 0.67, 95% CI: 0.51-0.88). A hazard ratio is a measure of how often an event (like death) happens in one group compared to another over time.
-
Impact on Recurrence: Women in the highest intake quartile had a 34% lower hazard of recurrence or breast cancer-related death compared to the lowest intake group (HR = 0.66, 95% CI: 0.52-0.84).
-
5-Year Rates: This translated to a multivariate-adjusted 5-year mortality rate of 9.2% in the highest soy intake group versus 13.1% in the lowest. The 5-year recurrence rate was 8.9% in the highest intake group versus 13.0% in the lowest.
Key Subgroup Findings (Addressing Clinical Concerns):
A primary concern regarding soy is that its estrogen-like isoflavones could promote cancer growth, especially in ER-positive tumors, or interfere with tamoxifen. This study directly addressed those concerns:
-
Estrogen Receptor (ER) Status: The inverse association (i.e., higher soy intake, lower risk) was seen in women with both ER-positive and ER-negative breast cancer.
-
Tamoxifen Use: The beneficial association was present in both users and non-users of tamoxifen. The study found that women with the highest soy intake had the lowest mortality and recurrence rates, regardless of their tamoxifen use.
Participants:
The analysis included 5,033 female breast cancer survivors from Shanghai, China. Participants were recruited approximately 6 months after their diagnosis.
Assertive Critical Appraisal
Limitations & Bias (STROBE Framework):
-
Confounding: This is the primary limitation. The authors report that women with high soy food intake also tended to have other healthy lifestyle habits, such as more exercise, higher intake of fish and vegetables, and lower intake of red meat. While the analysis statistically adjusted for many of these factors (e.g., exercise, other dietary intake, chemotherapy, disease stage) , “residual confounding resulting from measurement errors or unmeasured lifestyle factors could not be entirely ruled out”.
-
Reverse Causation: The authors considered the possibility that women with poorer health (perhaps from subclinical recurrence) might have reduced their food intake, making it look like low soy intake led to a bad outcome. They argue this is unlikely because intake of other foods, like meat, was not associated with survival, which would be expected if a general loss of appetite was the cause.
-
Short Follow-up: With a median follow-up of 3.9 years, the study “is still relatively short”. This prevents an evaluation of the long-term effects of soy intake.
Reporting Quality Assessment (STROBE):
The authors met key reporting standards by clearly describing their efforts to address confounding. They provided a comprehensive list of clinical predictors (e.g., TNM stage, ER status, tamoxifen use) and lifestyle factors (e.g., other dietary intake, physical activity) that were included in their statistical models to help isolate the effect of soy intake.
Applicability:
The findings are most directly applicable to Chinese women, whose average soy isoflavone intake (47 mg/day in this study) is “substantially higher” than that of US women (1-6 mg/day). Therefore, it is unclear if these benefits would apply to populations with different genetic backgrounds and much lower typical soy consumption.
Research Objective
The study’s objective was to evaluate the association of soy food intake after a breast cancer diagnosis with total mortality and cancer recurrence.
Study Design
This was a large, population-based prospective cohort study called the Shanghai Breast Cancer Survival Study. Data on lifestyle, diet, and disease progression was collected from 5,042 women at baseline (approx. 6 months post-diagnosis) and at follow-up interviews at 18, 36, and 60 months. Soy food intake was assessed using a validated food frequency questionnaire and was treated as a time-dependent variable, meaning the analysis could account for changes in a patient’s diet over the follow-up period.
Setting and Participants
The study was conducted in Shanghai, China. It included 5,033 women, aged 25-70, who had been diagnosed with primary breast cancer between 2002 and 2006 and had received surgical treatment.
Bibliographic Data
-
Title: Soy Food Intake and Breast Cancer Survival
-
Authors: Xiao Ou Shu, MD, PhD, et al.
-
Journal: JAMA
-
Year: 2009
-
DOI: 10.1001/jama.2009.1783
Mandatory Disclaimer: This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
Full text: PubMed Central
