Comment:
This 10-year follow-up of the PRIME II trial reinforces a crucial point for managing older patients with low-risk, hormone-positive breast cancer.
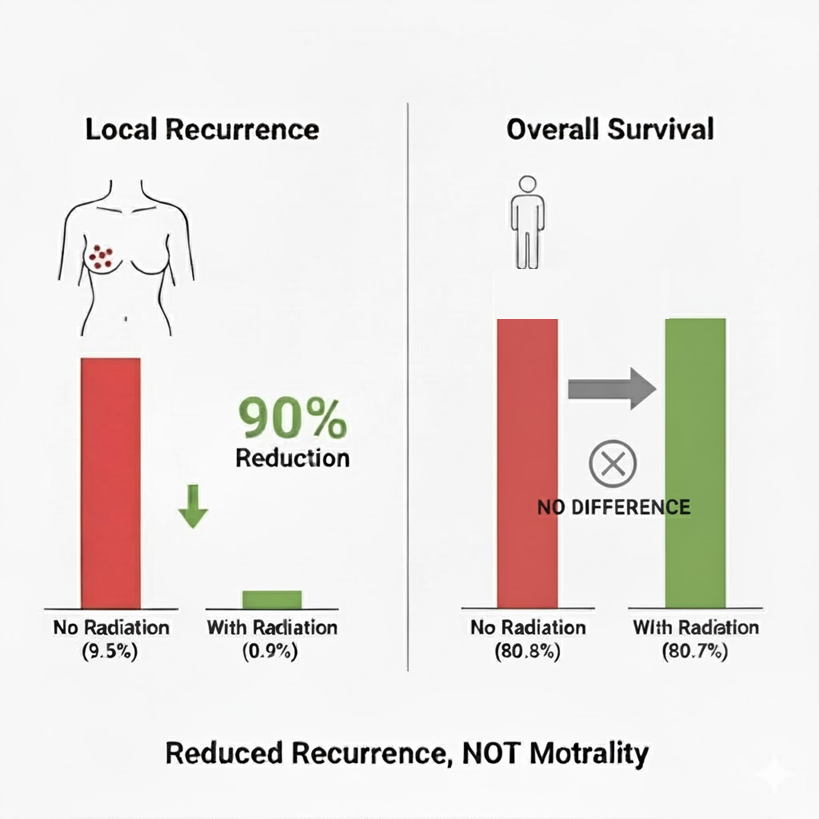
Yes, omitting radiotherapy after breast-conserving surgery increased the 10-year local recurrence rate significantly (from 0.9% to 9.5%). However, the definitive, practice-changing finding is that this 10-fold increase in local recurrence had zero impact on 10-year overall survival (OS) (80.8% vs. 80.7%). Similarly, there was no change in breast cancer-specific survival or distant recurrence.
For this specific population—women over 65 with low-risk disease—local recurrence is a surrogate endpoint, not a survival endpoint. The data shows that even if the cancer comes back locally, the disease is so indolent and treatable at that stage that it doesn’t shorten the patient’s life.
Some patients may still choose to do the radiation as they don’t want to have to go through local treatment again, but they need to be informed that it doesn’t impact anything beyond that.
Summary:
🩺 Clinical Bottom Line
This study provides strong 10-year follow-up evidence that for women 65 or older with low-risk, hormone receptor-positive, node-negative early breast cancer, omitting radiotherapy after breast-conserving surgery leads to a significantly higher risk of local recurrence.
However, and most critically, this increase in local recurrence did not translate into any detrimental effect on 10-year overall survival, distant recurrence, or breast cancer-specific survival. The 10-year overall survival was nearly identical (80.8% without radiotherapy vs. 80.7% with radiotherapy). These findings empower clinicians to discuss the omission of radiotherapy with eligible patients, balancing the avoidance of radiation’s harms against a higher, though still modest, risk of local recurrence.
📊 Results in Context
Primary Outcome
The primary endpoint was local breast cancer recurrence.
-
At 10 years, the cumulative incidence of local recurrence was 9.5% in the no-radiotherapy group.
-
This was significantly higher than the 0.9% incidence in the group that received radiotherapy.
-
The hazard ratio (HR) was 10.4 (95% CI, 4.1 to 26.1), meaning the hazard of a local recurrence was over 10 times higher in the group that omitted radiotherapy.
Key Secondary & Specialized Outcomes
-
Oncology Endpoints & Response Criteria: The central finding of this trial is the disconnect between the surrogate endpoint (local recurrence) and the gold-standard endpoint (overall survival).
-
Overall Survival (OS): This is the most important endpoint for demonstrating true clinical benefit. After 10 years of follow-up, there was no difference in overall survival between the two groups.
-
No Radiotherapy: 80.8% (95% CI, 77.2 to 84.3)
-
Radiotherapy: 80.7% (95% CI, 76.9 to 84.3)
-
-
Breast Cancer-Specific Survival (BCSS): Similarly, survival from breast cancer was almost identical at 10 years: 97.4% (no radiotherapy) vs. 97.9% (radiotherapy). This highlights that in this older population, most deaths were from causes other than breast cancer.
-
Distant Recurrence: Omitting radiotherapy did not increase the 10-year risk of the cancer spreading. The incidence of distant recurrence as the first event was 1.6% (no radiotherapy) and 3.0% (radiotherapy).
-
Patient-Reported Outcomes (PROs): This 10-year follow-up paper did not collect data on the toxic effects of radiation.
Harms and Adverse Events
The primary “harm” reported in this paper for the no-radiotherapy group was the 8.6 percentage-point increase in the absolute risk of local recurrence at 10 years. Data on radiation-specific complications (e.g., cardiac events, second cancers) were not collected in this trial.
🧐 Assertive Critical Appraisal
-
Risk of Bias (RoB 2 Framework): The overall risk of bias is low. This was a large, well-conducted, multicenter phase 3 randomized trial. Randomization was computerized and the analysis was performed on an intention-to-treat basis. While blinding was not possible (patients and doctors knew who received radiation), the primary endpoint (local recurrence) and survival outcomes are objective, minimizing the risk of bias from the open-label design.
-
Subgroup Analyses: A pre-specified exploratory analysis found that patients with ER-high tumors (the vast majority of the trial) who omitted radiotherapy had a 10-year local recurrence rate of 8.6%. In contrast, the small number of patients with ER-low tumors had a much higher 19.1% recurrence rate when omitting radiotherapy. This suggests the strategy of omitting radiotherapy is safest in the target population of ER-high cancers.
-
Reporting Quality Assessment (CONSORT): The reporting quality is high. The paper includes a complete CONSORT flow diagram detailing participant allocation and follow-up (Fig. 1). The methods for randomization and the statistical analysis plan are clearly described.
🎯 Applicability
The findings of this trial are highly applicable to daily clinical practice. The patient population—women aged 65 or older with low-risk (HR-positive, N0, T1/T2, Ω 3 cm) breast cancer—is very common. This study provides robust, long-term data to support a shared decision-making conversation about omitting whole-breast irradiation, a treatment that involves significant time, cost, and potential side effects.
📝 Research Objective
The trial’s objective was to determine if omitting whole-breast irradiation was detrimental to women 65 or older with low-risk, hormone receptor-positive early breast cancer who were receiving breast-conserving surgery and adjuvant endocrine therapy. The primary endpoint was local breast cancer recurrence.
🔬 Study Design
-
Type: A phase 3, multicenter, randomized, open-label, parallel-group trial (known as PRIME II).
-
Allocation: 1326 patients were randomized in a 1:1 ratio.
-
Intervention Group (n=668): Assigned to receive no irradiation after surgery and adjuvant endocrine therapy.
-
Control Group (n=658): Assigned to receive whole-breast irradiation (40 to 50 Gy) after surgery and adjuvant endocrine therapy.
🌍 Setting and Participants
-
Setting: 76 centers in the United Kingdom, Greece, Australia, and Serbia.
-
Participants: 1326 women.
-
Key Inclusion Criteria: Women 65 years of age or older; T1 or T2 primary breast cancer (tumor size ≤ 3 cm); node-negative; hormone receptor (ER or PR)-positive; treated with breast-conserving surgery with clear excision margins; and receiving adjuvant endocrine therapy.
📚 Bibliographic Data
-
Title: Breast-Conserving Surgery with or without Irradiation in Early Breast Cancer
-
Authors: Ian H. Kunkler, Linda J. Williams, Wilma J.L. Jack, David A. Cameron, and J. Michael Dixon
-
Journal: The New England Journal of Medicine
-
Year: 2023
-
DOI: 10.1056/NEJMoa2207586
This AI-generated analysis is for informational and research purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a qualified health provider with any questions you may have regarding a medical condition.
Original Article:
Full text here.
